Blood in Stool: Understanding the Basics
I’ll never forget the first time I noticed blood in my stool. Honestly, I thought I was dying. My mind raced from “Is this serious?” to “Maybe it’s just something small.” It’s a scary thing to see, especially when you don’t know what’s going on.
Finding blood in your stool means there’s bleeding somewhere along your digestive tract. It could be something as minor as a tiny tear near your anus or something more serious happening deeper inside your body.
Most of the time, the blood is coming from a simple issue like hemorrhoids or a small cut called an anal fissure. These usually happen when you’re constipated and pushing too hard during a bowel movement. I experienced that once after eating way too much cheese and barely drinking water. Not a great combo, trust me.
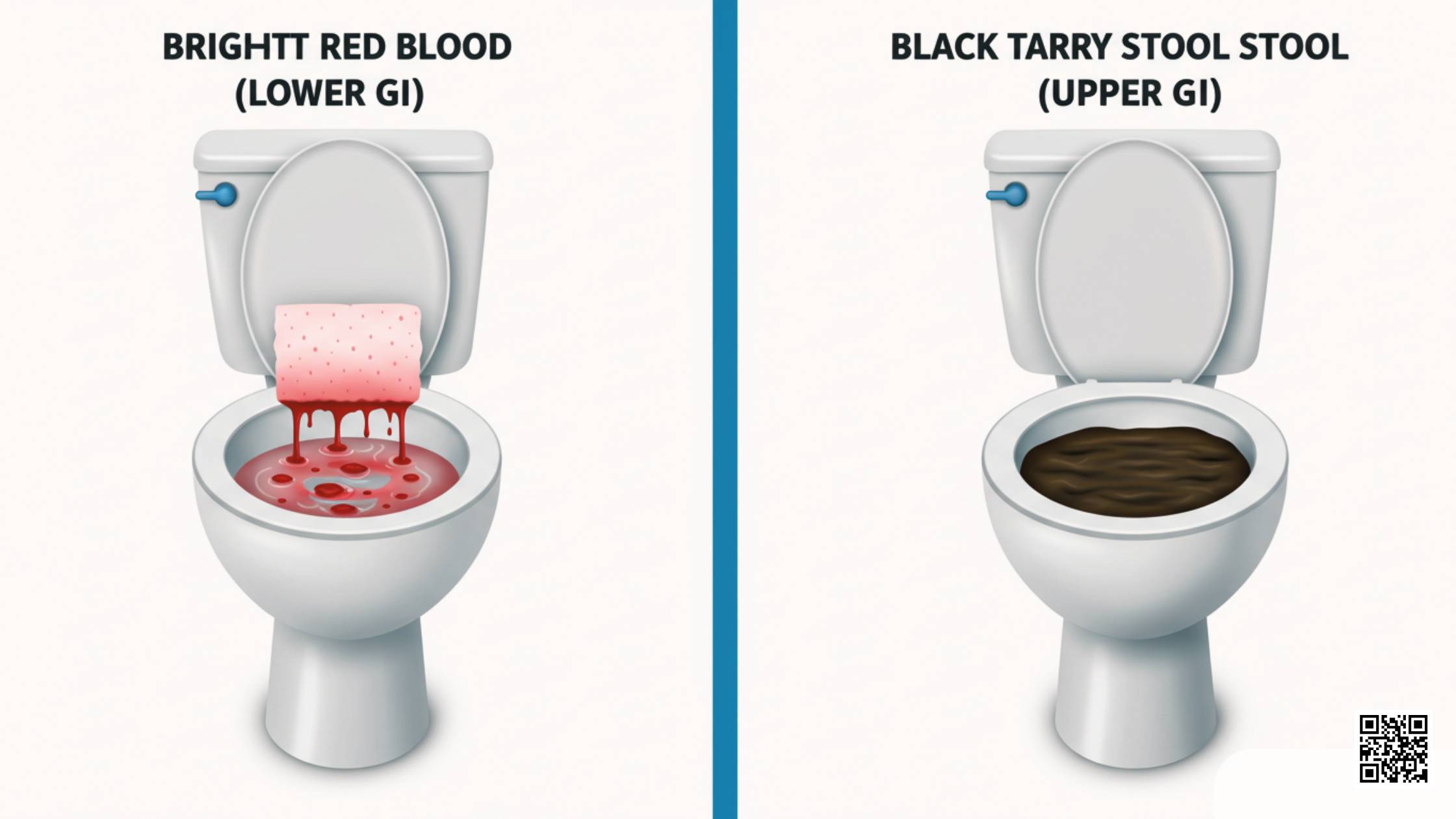
But sometimes, blood in stool can be a sign of a bigger problem. Conditions like colorectal cancer, inflammatory bowel disease (IBD), or ulcers can also cause bleeding. I always tell people, if the blood looks dark, sticky, or tar-like, it’s usually coming from higher up in your system — and that needs quick attention.
On the other hand, if the blood is bright red, it often means the bleeding is closer to the exit, like from the rectum or anus. That’s what happened in my case — bright red streaks, not dark clots, which my doctor said was “better news” if you can even call it that.
So, if you’re wondering why blood in stool happens or asking yourself, “Why do I have blood in my stool?”, know that it ranges from small, everyday problems to things that need a doctor right away. Either way, it’s your body’s way of waving a little red flag and saying, “Hey, look over here!”
Keeping an eye on the color, amount, and how often it happens can really help you figure out whether you’re facing a tiny issue or something that needs serious checking.
And just between you and me — no one ever regrets getting it checked out early. Waiting only makes you worry more.
When to Worry About Blood in Stool
When I first saw blood, I tried to tell myself it was nothing. But deep down, I couldn’t shake the worry. After all, how do you really know when blood in stool is serious and when it’s not?
If you ever see bright red blood just once and it’s a small amount, it might not be a big deal. Things like hemorrhoids or straining too hard can cause that. I’ve been there after a week of eating junk and not drinking enough water. Lesson learned.
But if the bleeding keeps happening, gets heavier, or if the blood looks dark, sticky, or tarry, that’s when you need to stop guessing and call a doctor. Dark blood usually means it’s coming from higher up in your digestive system — and that’s never something to ignore.
I remember asking my doctor, “How much blood should I actually be worried about?” He said, even small amounts can be a big deal if they show up again and again. It’s not just about the size; it’s about the pattern.
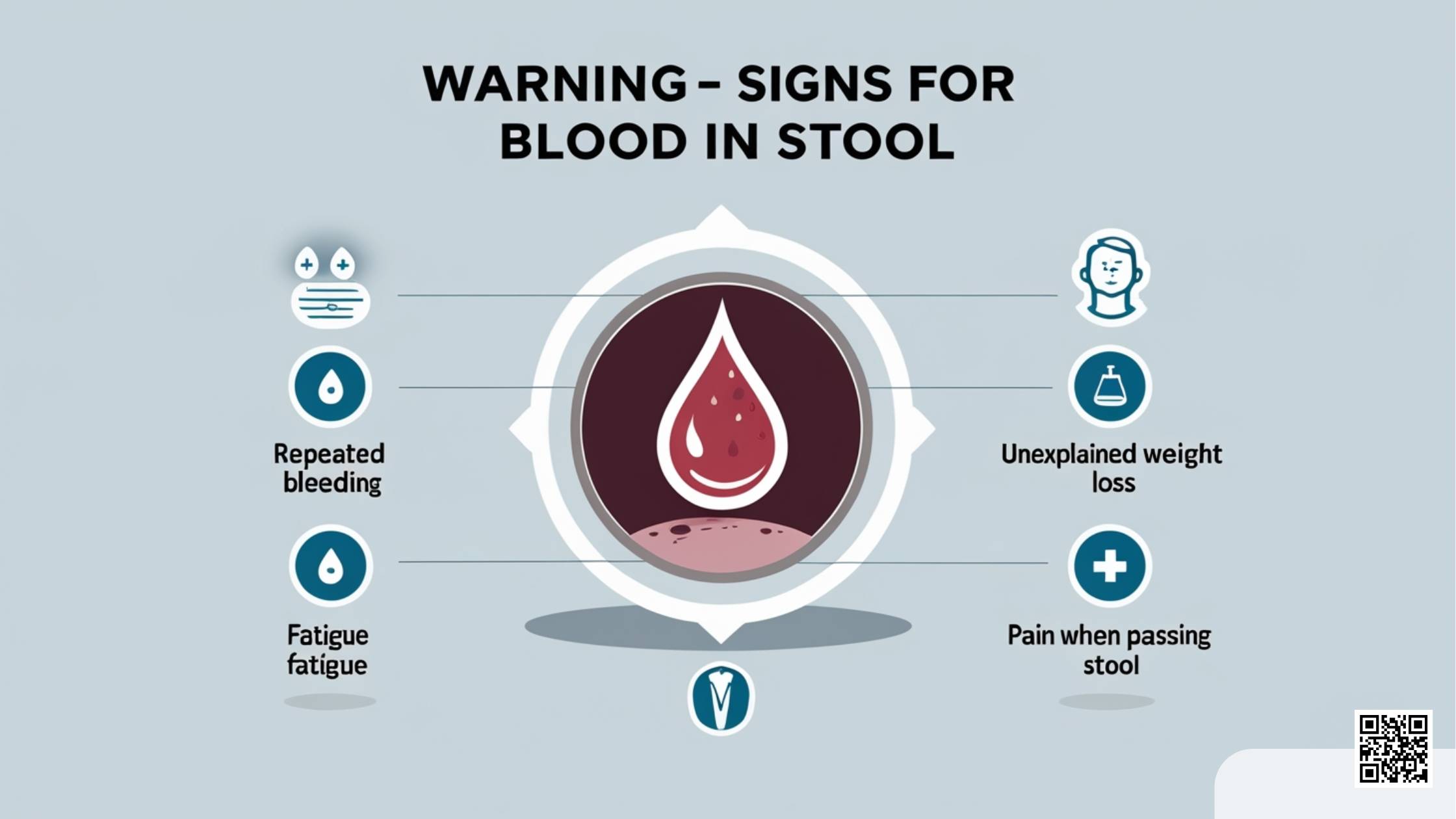
Another thing I didn’t realize at first was how important other symptoms are. If you feel pain when passing stool, that’s a clue that something could be wrong close to the rectum, like a fissure or hemorrhoids. I had sharp pain once that made me dread going to the bathroom, and trust me, that’s not normal.
Fatigue is another sneaky sign. If you’re bleeding inside your gut for a while, even tiny amounts, you can lose iron and start feeling drained all the time. I used to think I was just tired from work, but it was actually low iron from slow, hidden bleeding.
Unexplained weight loss is also a red flag. If the pounds are dropping off and you’re not even trying, something bigger could be going on. I lost about eight pounds without changing anything, and that was the moment I knew I couldn’t put it off anymore.
So, if you’re seeing bright red blood in your stool, having pain when passing stool, feeling wiped out, or losing weight without a reason — don’t just hope it will go away. These are signs that it could be serious, and the sooner you catch it, the better.
I used to be the king of “It’s probably nothing.” Now, if my body sends me a warning, I listen the first time.
Book an Appointment Now
Take the first step toward better gut health with Dr. Gina Sam. Personalized care is just a click away!
Book NowBlood When I Wipe but Not in Stool: What It Means
One morning, I wiped and noticed blood on the toilet paper. My heart jumped into my throat. I checked the stool itself, but there was no blood in it. I sat there wondering if I was about to discover something terrible.
There’s a big difference between blood in your stool and blood when wiping but not in stool. If you see blood on the paper but not mixed into your poop, it usually means the bleeding is happening right at the end — near the anus. It’s like having a scrape on your skin rather than something deeper inside.
The most common reasons for this are hemorrhoids and anal fissures. Hemorrhoids are swollen blood vessels that can pop up from straining during bowel movements. I got my first hemorrhoid after a long road trip where gas station food and zero water were my main diet. Not my proudest moment.
Anal fissures are tiny tears in the skin around the anus. They sound small, but they can feel like you’re sitting on broken glass. I still remember wincing every time I sat down after a hard bowel movement caused a fissure. It’s funny how something so small can ruin your whole day.
Now, should you worry if there’s no blood in the stool itself? Most of the time, if it’s just a few streaks on the paper and it goes away after a day or two, it’s not something urgent. I learned that minor bleeding from wiping too hard or passing a dry stool can happen to anyone.
But — and this is important — if the blood keeps showing up, if it gets heavier, or if you notice pain that doesn’t get better, don’t brush it off. That’s your body asking for help. After dealing with it more than once, I realized it’s way better to get it checked early than sit around making worst-case scenarios in your head.
Bottom line: a little blood when wiping might not be serious, but your body isn’t just throwing red flags for fun. Pay attention, stay calm, and don’t be afraid to get an expert’s opinion if it sticks around.
Blood When I Wipe but Not in Stool and No Pain: Should I Be Concerned?
I still remember how confused I felt the first time I wiped, saw blood, but felt no pain at all. Part of me thought, “Well, if it doesn’t hurt, maybe it’s no big deal.” Another part of me couldn’t stop worrying.
When you have blood when you wipe but not in your stool and no pain, it usually points to a few harmless reasons. The most common one is internal hemorrhoids. These little troublemakers can swell up inside the rectum and bleed, but because there aren’t many pain nerves inside there, you might not feel a thing. It’s kind of like having a silent protest happening in your body.
Another reason could be a very tiny anal fissure that’s healing. Sometimes a fissure isn’t deep enough to trigger pain but can still cause light bleeding when you wipe. I had that once after dealing with a stubborn case of constipation. No pain, just a little surprise on the toilet paper.
Mild irritation from wiping too hard can also cause painless bleeding. After a rough weekend of eating nothing but spicy wings, my digestive system made sure I regretted every single bite — and the wiping didn’t help either.
But even when there’s no pain, blood is still your body’s way of saying something’s off. So, when should you see a doctor? If you notice the blood sticking around for more than a few days, or if it gets heavier instead of lighter, it’s smart to get it checked out. I used to think I could out-stubborn my health issues, but that plan never really worked out for me.
Also, if the blood shows up with other signs like changes in your stool color, weird fatigue, or weight loss, don’t sit on it (pun not intended). Those could be clues that something deeper is going on.
To keep it simple: no pain doesn’t always mean no problem. Trust your gut — literally. If anything feels off or keeps happening, it’s better to be safe than sorry.
Bright Red Blood in Stool: Is It Serious?
The first time I saw bright red blood in the toilet, my stomach dropped. It looked so fresh that I thought something inside me must have just burst. I stood there wondering if I should sprint to the hospital or pretend it didn’t happen.
Bright red blood usually means the bleeding is coming from the lower part of your digestive tract — the rectum or the anus. Because the blood hasn’t traveled far, it stays red and fresh-looking. It’s kind of like getting a small cut on your skin; the blood is right there, still full of oxygen.
When the blood is this bright, it’s often linked to minor causes like hemorrhoids or small tears called anal fissures. I once got hemorrhoids after a few too many days of skipping fiber and living off sandwiches. Let’s just say, my bathroom visits turned into mini panic attacks for a week.
But here’s the thing: bright red blood isn’t always harmless. Sometimes it can point to more serious problems like polyps in the colon or even colorectal cancer. Polyps are little growths that can bleed, and if ignored, they can turn into something much worse. When I found that out during a late-night Google spiral, I couldn’t sleep until I booked a check-up.
The tricky part is, minor and serious causes can look pretty similar on the surface. That’s why patterns matter. If you see bright red blood once after a tough bowel movement, it could just be from straining. I’ve been there — white-knuckling it through constipation and then spotting a little blood afterward.
However, if the bleeding keeps happening, or it comes with other signs like pain when passing stool, fatigue, or even feeling like you didn’t completely empty your bowels, that’s when you need to act fast. No WebMD guessing games — just real doctor answers.
I learned the hard way that waiting it out doesn’t make problems disappear. If anything, it makes the anxiety grow until you’re diagnosing yourself with every disease under the sun. Fun times, right?
So to wrap it up: a one-off streak of bright red blood might not be a reason to panic. But if it becomes a regular guest appearance, don’t shrug it off. Trust me, peace of mind is way better than wondering “what if” every time you head to the bathroom.
Blood in Toddler’s Stool: When to Worry
Seeing blood in my toddler’s stool for the first time was one of those moments where I almost dropped everything and rushed to the ER. There’s something about your kid being in trouble that hits a different level of panic.
Most of the time, blood in a toddler’s stool comes from something small and fixable. Constipation is one of the biggest reasons. When little kids get backed up, their stool can become hard and dry. Pushing out a hard stool can cause tiny tears around the anus, called anal fissures. I’ve seen this happen after a week of my kid refusing to eat anything but bread and cheese.
Sometimes, it’s hemorrhoids too. Even though we think of hemorrhoids as an adult thing, toddlers can get them if they strain hard during bowel movements. It’s not super common, but it happens — and let me tell you, trying to explain hemorrhoids to a three-year-old isn’t exactly easy.
Infections can also cause blood in the stool. Things like bacterial or viral stomach bugs can irritate the lining of the intestines and cause a little bleeding. I remember after a rough stomach flu, my son had diarrhea with a few streaks of blood. The doctor said it was the infection irritating his gut and that it would clear up once the virus was gone.
Now, when does it get serious? If you see a lot of blood, or if the bleeding doesn’t stop after a few days, that’s a red flag. Another time to worry is if the blood is dark or mixed into the stool, not just on the outside. That can sometimes point to bleeding higher up in the intestines.
You should also watch out if your toddler has other symptoms like a high fever, acting super tired, losing weight, or having bad belly pain. Those can point to bigger issues like inflammatory bowel disease (IBD) or even a food allergy that’s causing inflammation inside the gut.
One thing I learned quickly: trust your gut when it comes to your kid. Doctors would always rather you come in and be wrong than stay home and miss something important. I’d much rather deal with a little embarrassment than risk my child’s health.
To sum it up, blood in a toddler’s stool is often not serious, but it’s never something to ignore. If the blood is heavy, dark, or paired with other worrying signs, it’s time to get help right away.
Blood in Baby’s Stool: What Parents Need to Know
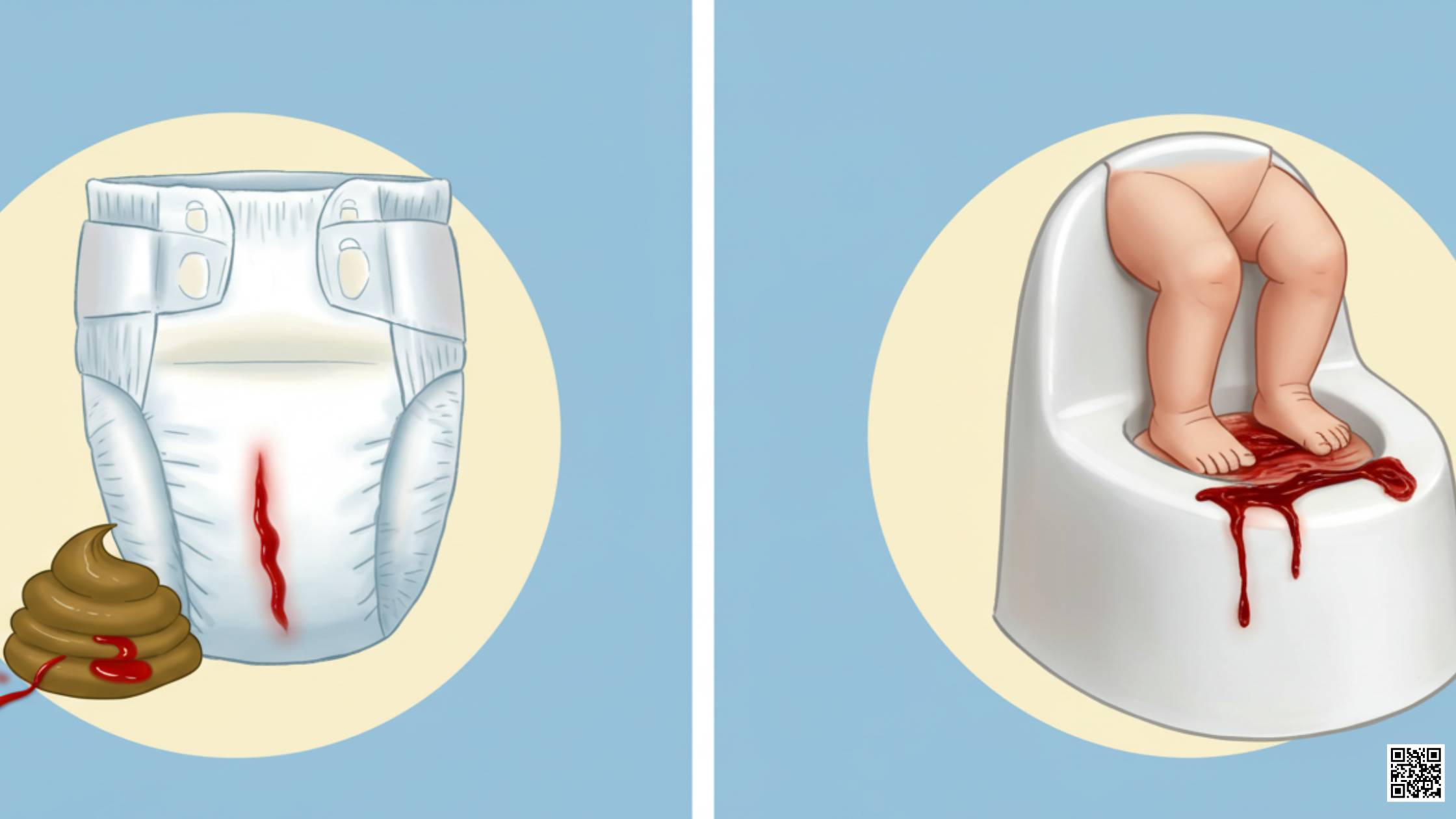
The first time I spotted blood in my baby’s diaper, my heart pretty much stopped. I must have stared at it for a good minute, wondering if I should call the doctor or an ambulance. When it’s your baby, even a little blood feels like a huge emergency.
In babies, one of the most common reasons for blood in the stool is a milk protein allergy. Sometimes their tiny bodies can react to cow’s milk proteins — even through breast milk — and this can cause irritation in their intestines, leading to little bits of blood. I found that out the hard way after a long night of crying, diaper changes, and googling every worst-case scenario imaginable.
Anal fissures are another big cause. Babies can get tiny tears around the anus, especially if they’re constipated or straining a bit during pooping. It’s painful to think about, but usually, it’s just a small tear that heals quickly once their poop softens back up. After one stressful episode, my pediatrician gently explained that it’s way more common than most new parents realize.
Now, here’s when you should really worry. If the blood is dark, looks like coffee grounds, or the stool turns black and tarry, that’s not normal. That can signal bleeding from higher up in the digestive tract, and it needs fast medical attention.
You should also be concerned if your baby seems really fussy, won’t eat, throws up, or shows signs of dehydration like dry lips or fewer wet diapers. I always tell new parents: if your gut feels uneasy, trust it. Babies can’t tell us what’s wrong, so you have to be their voice.
Another huge sign is if the bleeding doesn’t stop or keeps showing up in multiple diapers. Even if the baby acts fine otherwise, repeated blood needs to be checked out. When it happened to us, the doctor ordered some simple tests and ruled out anything serious — but getting those answers made a world of difference.
In short, blood in a baby’s stool might be something small like a milk protein allergy or a minor tear, but it should never be ignored. When it doubt, call your pediatrician. It’s always better to feel a little silly than to regret waiting too long.
Blood in Cat’s Stool: When to Worry
I never thought I’d be the type of person to inspect cat poop, but the day I spotted blood in my cat’s litter box, I became one. It caught me off guard. One minute my cat was acting normal, the next minute I was panicking over a few drops of red in the clumps.
Cats can have blood in their stool for a bunch of reasons, and not all of them are scary. Sometimes it’s something small, like constipation. If they strain too hard to poop, it can cause tiny tears that bleed. My cat, being the drama queen she is, managed to get constipated after refusing to drink water for days because she didn’t like her new bowl. True story.
Diet changes can also upset their stomachs. Switching food too quickly can cause inflammation and some bleeding. I learned the hard way that “new food excitement” isn’t worth it if you’re not easing it in slowly.
Parasites like worms can also be to blame. They irritate the intestines and can cause bleeding. It’s gross to think about, but after my vet explained it, I realized how easy it is for indoor cats to pick up parasites just from tracking dirt inside.
But when should you really worry about blood in your cat’s stool? If the bleeding is more than a few drops, happens more than once, or if the stool looks black and sticky (which points to bleeding higher up), you should call the vet right away.
Also, if your cat is acting weird — like hiding, not eating, vomiting, or losing weight — that’s a major red flag. Cats are experts at pretending they’re fine until they’re really not. I learned quickly that by the time a cat shows they’re sick, it’s usually serious.
Another thing to watch for is straining in the litter box. If you notice your cat making several trips but not producing much or crying when trying to poop, don’t wait around. When this happened with my cat, I rushed her to the vet and found out she had a bad case of colitis. A few medications later, she was back to bossing me around like usual.
In short, blood in a cat’s stool might be from simple things like constipation or a minor irritation, but it can also mean bigger problems. When in doubt, get your furry boss checked out. They might not thank you now, but they’ll be purring later.
Common Causes of Blood in Stool: Why It Happens
After that first scare with blood in my stool, I found myself asking the same question over and over: Why do I have blood in my stool? I needed real answers, not just scary headlines from internet searches.
Turns out, there are a lot of reasons why blood in stool happens. Some are small fixes. Some need serious medical help. Knowing the difference can save you a lot of stress — and maybe even your life.
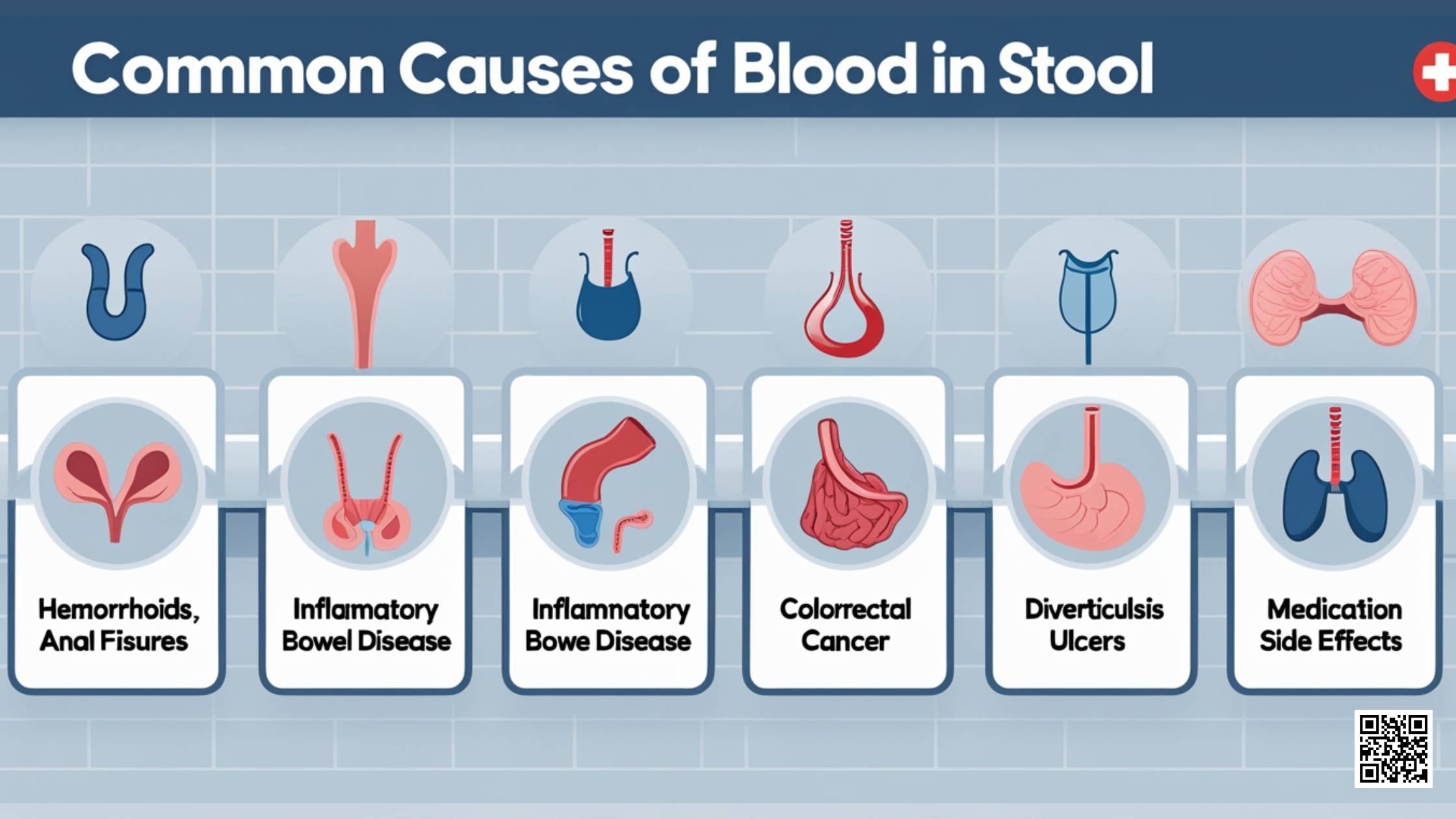
One of the most common causes is hemorrhoids. These are swollen veins in your lower rectum or anus. They can bleed when you strain too hard during a bowel movement. I got a bad case once after a week of bad eating habits and pretending coffee was an actual meal. Spoiler alert: it’s not.
Anal fissures are another reason. These are tiny cuts around the anus caused by passing hard or large stools. They hurt — a lot. It feels like passing glass, not poop. The first time I had one, I thought something had seriously torn inside me, but thankfully, it was just a small tear that healed with some fiber and patience.
Diverticulosis is a little sneakier. It’s when small pouches form in your colon wall. Sometimes they can bleed without much warning. I didn’t know about diverticulosis until a family member had a sudden bleeding episode that led to a hospital visit. One day fine, next day a lot of blood.
Then there’s the big scary one — colorectal cancer. I won’t sugarcoat it. Blood in the stool can sometimes be a sign of cancer in the colon or rectum. It doesn’t always come with pain either, which makes it even trickier. That’s why catching any new bleeding early is so important.
Inflammatory Bowel Disease (IBD), like Crohn’s disease or ulcerative colitis, can also cause bleeding. These conditions make your digestive system inflamed and raw, leading to blood. IBD is serious and usually comes with other symptoms like stomach pain, weight loss, and diarrhea.
If you’ve ever had gastroenteritis — basically a stomach bug — you might have noticed some blood too. Severe diarrhea can make your intestines angry enough to bleed a little. After a brutal food poisoning trip, I learned that you can survive on nothing but crackers and regret for three days straight.
Lastly, some medications can make bleeding more likely. NSAIDs like ibuprofen, or blood thinners like warfarin, can cause small bleeds in your stomach or intestines. My granddad had to switch medications because even though he felt fine, his stools started showing streaks of blood.
So if you’re sitting there wondering why do I have blood in my stool, the answer could be something simple — or something that needs quick action. Either way, don’t ignore it. Your bathroom habits are telling you more than you think.
Pain When Passing Stool and Blood: Linked Causes
Out of all the things I’ve felt in my life, pain when passing stool is high on the “never want to repeat” list. It’s not just uncomfortable — it’s the kind of pain that makes you rethink every meal you’ve ever had.
Most of the time, straining and constipation are the main villains behind it. When you’re pushing way too hard because your stool is hard or dry, you put a lot of pressure on the tissues around your anus. I once went three full days without a proper bowel movement. Let’s just say by day four, things got ugly — and bloody.
Straining can cause hemorrhoids to swell or even burst a little, leading to blood on the toilet paper or in the bowl. It can also create anal fissures, those tiny but brutal tears in the skin that feel way bigger than they look. Every time I sat down after my first fissure, I felt like I was being betrayed by my own body.
Constipation doesn’t just cause pain; it sets the whole stage for injury. The longer poop stays stuck inside you, the harder and sharper it gets. Then when you finally manage to go, it scrapes and tears the tissues — a bad ending to an already bad experience.
Now, here’s when pain plus blood becomes a real red flag. If the pain is sharp, doesn’t go away, or keeps happening every time you go, it’s not just “normal constipation.” I made the mistake once of ignoring it for weeks. It turned out I had a bigger problem brewing that needed actual treatment, not just “drink more water” advice.
Another sign it’s serious? If you feel a heavy, throbbing pain after you poop, or if you notice swelling, lumps, or constant irritation around the anus. These signs can point to infections, abscesses, or worse. And if you ever get fever along with the pain and bleeding, that’s your cue to stop waiting and get medical help immediately.
Honestly, there’s no prize for toughing it out. Pain while pooping and seeing blood are two things your body does NOT do just for fun. If it hurts more than once or sticks around, it’s time to call someone who actually knows how to fix it.
If I learned anything the hard way, it’s this: your butt deserves better.
When to See a Doctor: Urgent Symptoms You Shouldn’t Ignore
At first, I thought ignoring the blood in my stool would make it disappear. I mean, if you don’t think about it, it’s not real, right? Wrong. That little red warning turned out to be something I should’ve acted on way sooner.
There are clear signs that tell you it’s time to stop guessing and see a doctor. If you’re wondering when to worry about blood in stool, here’s a quick checklist I wish I had memorized earlier:
- Bleeding that lasts more than a day or two
- A lot of blood (not just a tiny streak)
- Dark, tarry stools (a sign of internal bleeding)
- Bright red blood in stool serious enough to pool in the toilet
- Pain when passing stool that doesn’t go away
- Unexplained weight loss
- Feeling tired all the time
- Belly pain that sticks around or keeps coming back
- Changes in bowel habits (like diarrhea or constipation that won’t quit)
- Feeling dizzy or lightheaded after going to the bathroom
If you check even one of these boxes, it’s not time to play it cool. It’s time to call a doctor. I waited way too long once because I thought I was being dramatic. Turned out, my body wasn’t trying to win an Oscar for Best Drama — it was genuinely asking for help.
Early diagnosis can make a massive difference. Small problems stay small if you catch them early. Hemorrhoids can be treated easily before they turn into a big painful mess. Tiny fissures can heal with simple changes instead of needing surgery later. And in the worst-case scenario, catching something serious like colorectal cancer early can literally save your life.
When I finally got checked out, it was a huge relief just to know what I was dealing with. No more sitting around imagining every possible horror story. If you’re seeing any of these symptoms, don’t wait like I did — visit Dr. Gina Sam, a trusted gastroenterologist, who knows exactly how to get to the bottom of digestive problems. You deserve real answers and real peace of mind.
Your body isn’t trying to annoy you. It’s trying to keep you alive. Listen to it the first time.
Diagnosis and Tests: How Doctors Find the Cause
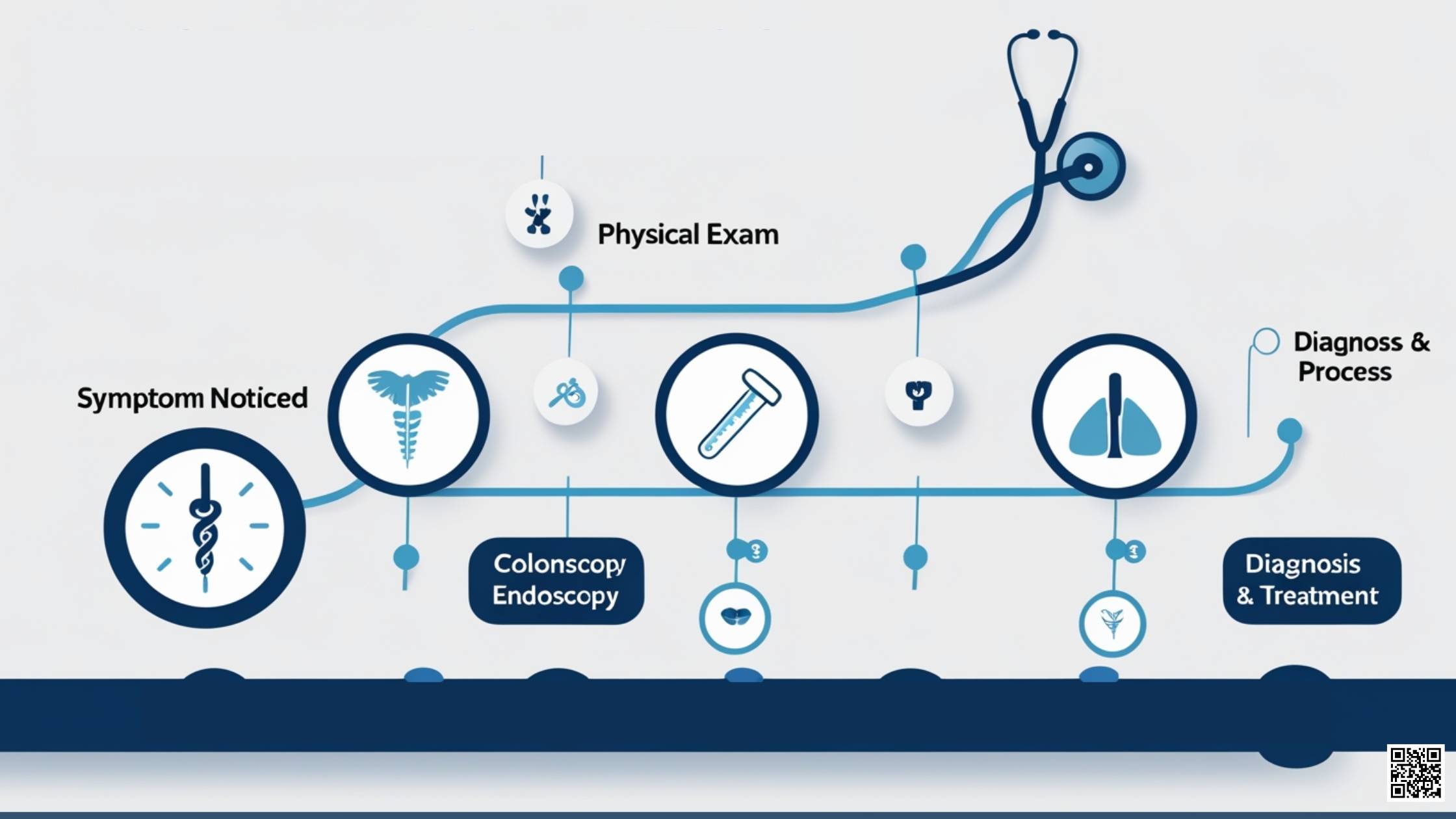
When I finally decided to stop being stubborn and saw a doctor about the blood in my stool, I realized something — figuring out what’s wrong isn’t as scary as you think. In fact, it was one of the smartest choices I made.
It all started with a physical exam. Nothing dramatic. The doctor asked me a lot of questions first — when I noticed the bleeding, how often it happened, if I had any pain when passing stool, and if anything else felt different. Talking about bathroom habits face-to-face wasn’t exactly on my bucket list, but honestly, they hear it all the time.
After that, the doctor did a quick external check. They looked for hemorrhoids, fissures, or anything obvious around the anus. I was nervous, but it took just a few minutes. Sometimes they might also do a simple rectal exam with a gloved finger to feel for swelling, growths, or tenderness.
Next, they ordered stool tests. That meant bringing in a small sample (fun times) to check for hidden blood, infections, or signs of inflammation. I thought it would be more complicated, but picking up a kit from the pharmacy and following instructions made it easy enough. Plus, no guessing games — the lab would pick up things my eyes couldn’t see.
When the stool test didn’t give enough answers, they recommended a colonoscopy. At first, just hearing that word made me want to run for the hills. But after talking to the team, I realized it wasn’t as bad as it sounded. I prepped the night before (yes, it was unpleasant, but doable) and then went in for the procedure. They used a tiny camera to look at my colon and rectum from the inside.
An endoscopy works similarly but is used to check the upper parts of your digestive system — like the esophagus and stomach. I didn’t need one, but a friend of mine who had different symptoms went through it and said it was surprisingly quick.
Through these tests, they found the real reason for my bleeding — and more importantly, they ruled out all the worst-case scenarios my brain had been cooking up. That alone was worth every awkward conversation and every uncomfortable prep drink.
If you’re worried about blood in stool or pain when passing stool, the truth is, figuring out the cause is way less scary than living with the unknown. I wish I hadn’t waited so long, but at least now I can say with full confidence: knowing is way better than wondering.
Treatment Options for Blood in Stool
After the tests were done and I finally knew what I was dealing with, the next big question hit me: How do I fix this? Thankfully, treating blood in stool isn’t always complicated, especially when you catch it early.
For me, it started with home treatments. My doctor explained that a lot of the smaller causes — like hemorrhoids or minor fissures — can get better just by changing what you eat. I was told to load up on fiber. At first, I thought fiber was just some boring cereal my grandma ate, but it turns out, it makes a huge difference. Foods like oatmeal, fruits, veggies, and beans became part of my everyday meals.
Drinking more water was another big change. I used to survive on coffee and soda without thinking twice. Now, I carry a water bottle almost everywhere. Staying hydrated keeps your stool soft, which means way less pain when passing stool — and a much lower chance of tearing something.
There were a few over-the-counter things that helped too. My doctor recommended stool softeners (not laxatives) when needed and a soothing cream to help with hemorrhoids. These small things made a massive difference in just a few days.
But sometimes, medical treatments are needed when home tricks aren’t enough. If hemorrhoids get too big, doctors might suggest simple procedures like rubber band ligation (where they tie off the hemorrhoid so it shrinks and falls off). It sounds brutal, but a friend of mine had it done and said it was way easier than he expected.
For anal fissures that don’t heal, stronger creams with prescription medicine help relax the muscles and give the tear a chance to heal. In rare cases, surgery is an option, but that’s usually the last resort.
When it comes to more serious causes like inflammatory bowel disease or polyps, treatment plans get a little more intense. Medications to calm inflammation, antibiotics for infections, or even surgeries to remove problematic areas might be needed. A good gastroenterologist, like Dr. Gina Sam, can guide you through every step if things get complicated.
I learned the hard way that pretending it would all magically heal didn’t get me anywhere. Following a real plan, sticking to it, and making simple changes helped me avoid bigger problems down the road.
If you’re dealing with blood in stool or pain when passing stool, don’t wait to make changes. Small steps can lead to major relief — and you’ll be back to feeling normal a lot faster than you think.
Preventing Blood in Stool: What You Can Do
After dealing with the nightmare of blood in stool and pain when passing stool, I realized something: it’s way easier to prevent the problem than to fix it later. Seriously, a few simple habits can save you a lot of pain, panic, and emergency Google searches at 2 AM.
First thing I changed was my diet. Eating a high-fiber diet is like giving your digestive system the tools it needs to work properly. Fiber keeps stool soft and easy to pass. I used to think fiber meant sad salads, but turns out, stuff like berries, apples, beans, and even popcorn are packed with it. Once I made fiber a regular part of my meals, bathroom trips got a whole lot easier — and a lot less terrifying.
Hydration was the next big game-changer. I used to drink water only when I was dying of thirst. Bad idea. Now, I aim to sip water throughout the day, not just during meals. Water keeps your stool soft and your gut moving smoothly. When I slack off and don’t drink enough, I can feel the difference — and not in a good way.
Another huge tip: avoid straining during bowel movements. Sounds simple, right? But when you’re rushing, stressed, or ignoring your body’s signals, it’s easy to push too hard. Straining leads to hemorrhoids and fissures, and trust me, you do not want to join that club. I started giving myself more time in the bathroom. No phones, no forcing it. Just patience.
Some days, if things weren’t moving, I’d add an extra fiber supplement like psyllium husk or take a short walk to get things going naturally. Movement helps your bowels stay active. Sitting all day, like I used to during long workdays, made everything worse.
I also learned not to ignore the urge to go. Holding it in just makes stool harder and drier, which sets you up for a painful time later. If your body says it’s time, it’s time.
The bottom line? Keeping pain when passing stool and blood in stool out of your life isn’t rocket science. It’s small choices every day — eat smart, drink water, move a little, and listen to your body.
I’m not perfect about it even now, but whenever I slip and start living off junk food and coffee, my body reminds me real quick who’s actually in charge.
FAQs (Frequently Asked Questions)
When I first dealt with blood in stool, my brain was overflowing with questions. I didn’t even know where to start. Here are the biggest ones I asked (and got real answers for).
Can blood in stool go away on its own?
Sometimes, yes. I had minor bleeding once from a small anal fissure, and it healed on its own after a few days of better eating and more water. If the bleeding is light, rare, and goes away quickly, it’s usually not a major crisis.
But if it keeps happening, gets heavier, or comes with other weird symptoms, it’s not something to just hope away. I learned the hard way that “waiting it out” isn’t a good plan for anything involving blood.
Is bright red blood always serious?
Not always. Bright red blood often comes from lower down — like hemorrhoids or a small tear — and most of the time, those are easy to treat.
I’ve had a few cases where it was just from straining too much after being constipated. No long-term issues, just a wake-up call to fix my habits.
That said, repeated or large amounts of bright red blood are never normal. If you keep seeing it, even if it’s bright, you should get it checked out. Better safe than sorry.
What should I do if my toddler or baby has blood in stool?
The day I found blood in my kid’s diaper, I went into full panic mode. But the doctor calmed me down and explained that in toddlers and babies, it’s often caused by things like constipation, anal fissures, or even food sensitivities like milk protein allergy.
If it’s just a tiny streak and the baby is otherwise acting normal, it might clear up fast. But if the blood is dark, heavy, or if your baby seems cranky, sick, or stops eating, that’s when you need to act.
If you ever wonder, when should I worry about blood in my baby’s stool, just trust your gut. When something feels off, don’t wait — call the doctor. That peace of mind is worth everything.
Should I be worried about blood when I wipe but not in stool?
I asked this exact question after my first scare. If you notice blood when you wipe but not in the stool itself, it usually points to something near the exit — like hemorrhoids or a small fissure. Especially if you’re seeing blood when wiping but not in stool and no pain, it often isn’t serious.
Still, if it keeps happening or the amount of blood increases, don’t brush it off. I had a period where I kept seeing small streaks for a few days straight, and my doctor found a small hemorrhoid that needed a little help healing.
Bottom line? If it’s once or twice and goes away, not a big deal. If it lingers or worsens, get it checked.
Reference and Citations:
- University Health Services, University of California, Berkeley. Hemorrhoids and Anal Fissures. Published 2010. https://uhs.berkeley.edu/sites/default/files/Hemorrhoids.pdf
- Sabry AO, Sood T. Rectal Bleeding. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK563143/






