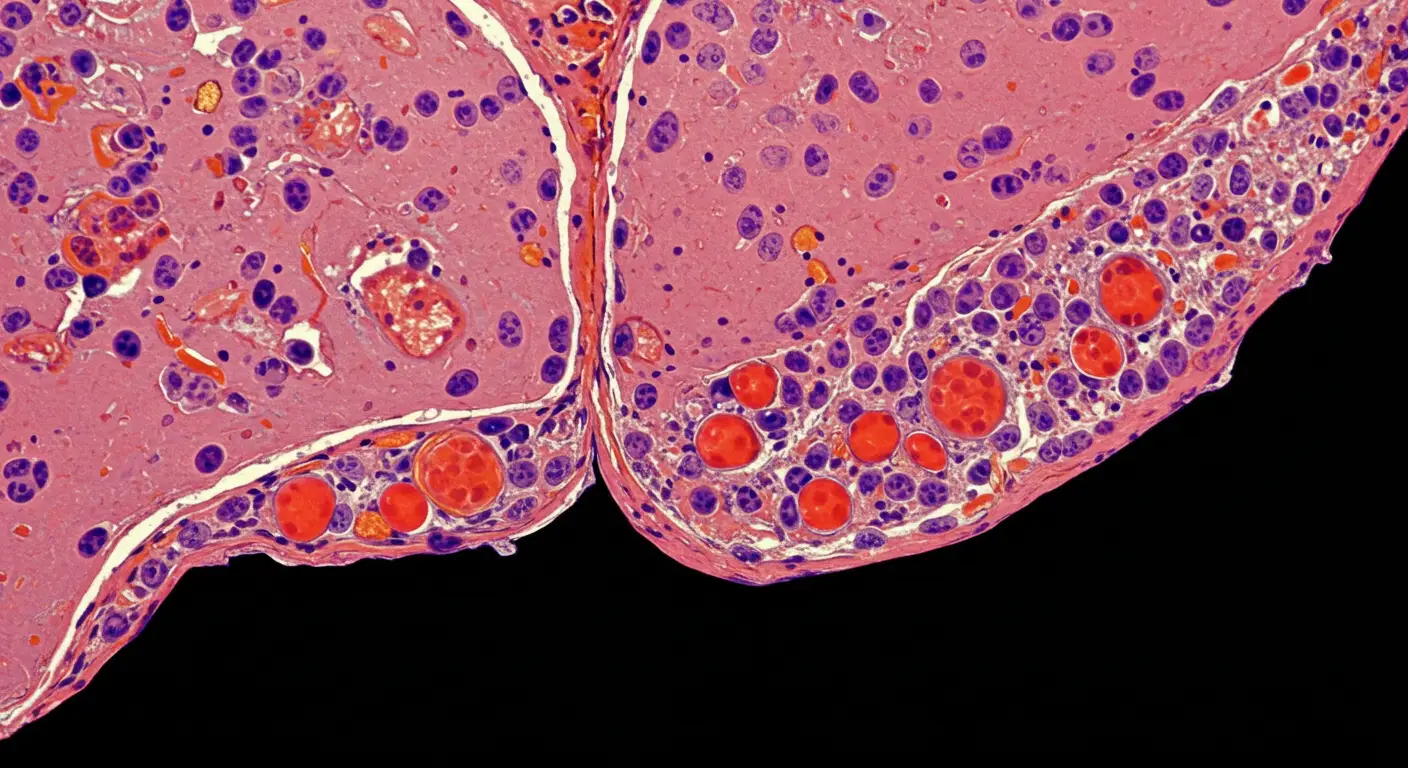
Cirrhosis is a pathologic process in the liver that is characterized by constant inflammation, fibrosis, and distortion of helical structure. Importantly, it is the most serious predisposing factor to hepatocellular carcinoma (HCC), which constitutes about 90 percent of all primary liver cancer.
The Centers for Disease Control and Prevention (CDC) confirm that in today’s America, the cases of HCC have tripled since 1980 and are closely intertwined phenomena with underlying cirrhosis instances. These relationships can play a crucial role in the work of health practitioners who want to make the care of their patients optimal by identifying, treating, and preventing diseases at the earliest possible moments.
Cirrhosis and Cirrhosis Oncogenic mechanism
There are a lot of misconceptions about the nature of cirrhosis and cancer that people must understand because they are only forcing a particular situation under this condition. This condition is a fact that people must learn about the nature of this condition and its oncogenic mechanism.
Cirrhosis comes about due to continued liver damage, usually by chronic viral hepatitis, chronic alcohol abuse, or metabolic disorders such as nonalcoholic fatty liver disease (NAFLD). Liver tissue would eventually turn into fibrotic, nodular tissue as hepatocytes continue to suffer damage and regenerate, taking place continuously.
This long-acting process activates the process of carcinogenesis in many ways:
- Long-term inflammation and oxidative stress also produce DNA mutation.
- Liver activation of hepatic stellate cells activates fibrogenesis and deposition of extracellular matrices.
- Imbalance in the cellular pathways, like Wnt/L-catenin, JAK/STAT, and TGF-l, promotes uncontrolled cell growth.
All these mechanisms provide a local environment that promotes malignant hepatocyte transformation.
Epidemiology: Quantifying the Risk
According to the American Cancer Society (ACS), more than 41,000 new liver cancer cases have been diagnosed in the U.S., 75 to 90 percent of which lived with the pre-existing cirrhosis. HCC annual incidence The proportion per year of HCC among cirrhotic patients varies with etiology:
- Hepatitis C Virus (HCV): 3 to 8 percent every year odds
- Hepatitis B Virus (HBV): 2-5 percent per year risk
- Alcoholic Liver Disease: Simple 2-4 percent a year risk
- NAFLD/NASH: Increasingly recognized as becoming a problem with a 1-3 percent annual risk for cirrhotic patients
Compensated cirrhosis (Child-Pugh Class A) patients still have rather well-conserved hepatic activity but still run a high risk of developing HCC.
Major Etiological Factors Increasing HCC Risk
1. Viral Hepatitis
- The causes of more than 50 percent of liver cancer in the world are attributed to chronic HCV and HBV infection. Even in patients who have attained virological suppression or deactivation, the trace of cirrhotic changes cannot be lost, and the surveillance of HCC is needed.
2. Alcohol Abuse
- Overuse and prolonged intake of alcohol increases the rate of liver fibrosis. CDC estimates that cirrhosis, which causes 47 percent of the deaths in the U.S., is alcohol-caused.
3. Non-alcoholic fatty liver disease (NAFLD)
- With an increasing number of obese and type 2 diabetic patients, NAFLD is gaining status as the most rapid cause of cirrhosis and HCC. About 20 percent to a quarter of NAFLD patients progress to non-alcoholic steatohepatitis (NASH), which is more aggressive and results in fibrosis and cirrhosis.
Screening and Surveillance Guidelines
Since cirrhosis is characterized by high oncogenic potential, it is important to detect the condition at an early stage during surveillance.
AASLD has the following recommendations:
Ultrasound with or without alpha-fetoprotein (AFP) measurement every six months on all cirrhotic patients, irrespective of the etiology of the disease.
Such a tactic has been proved to:
Diagnose HCC at an early point when it may still be curable.
Improve survival in general, and 5-year survival could reach up to 70-80 after the early intervention.
Indeterminate lesions or patients with high needs might be taken through advanced imaging modalities such as MRI and CT scans.
Treatment Strategies for HCC in Cirrhotic Patients
The multidisciplinary approach is required in the issue concerning the management of HCC in the condition known as cirrhosis. The treatment is based on the stage of tumors, liver functions, and the performance status of the patients as follows:
Curative Treatments:
- Surgical Resection: a favorite option when patients have early-stage HCC and intact liver functions.
- Liver Transplantation: Patients with Milan Criteria (single 5 cm or 3-3 cm multi-nodules) should undergo transplant, which has a curative effect with the elimination of underlying cirrhosis.
Locoregional Therapies:
- Radiofrequency ablation (RFA): This works on tumors 3 cm in size or smaller.
- Transarterial Chemoembolization (TACE): The intermediate stages of tumor are recommended.
Systemic Therapies:
- Sorafenib and the newer lenvatinib are targeted therapies that can also produce a survival advantage in advanced-stage disease, as can immunotherapies, such as atezolizumab and bevacizumab.
Preventive Approaches
Prevention strategies aim at management of the underlying liver diseases:
- Antiviral therapy (DAA therapy of HCV, nucleos(t)ide antivirals of HBV) decreases the rates of fibrosis and the risk of HCC dramatically.
- Lifestyle interventions: Weight loss, diabetic management, and alcohol withdrawal are essential in NAFLD and alcoholic liver disease subjects.
- Administration of HBV Vaccination is considered a leading form of preventative intervention, especially among vulnerable groups.
Emerging Advances in Risk Stratification
Innovative studies are emerging to combine biomarkers (AFP-L3, des-gamma carboxy prothrombin), genomic profiling, and AI-augmented imaging in personalized risk assessment and early detection of HCC among activities on the cirrhotic target population. Such innovations can enhance levels of surveillance and customization of treatments.
Conclusion
Cirrhosis greatly increases the possible risk of hepatocellular carcinoma due to chronic damage occurring to the liver and fibrotic reconstruction, which facilitates carcinogenesis. Medical workers should acknowledge cirrhosis as the key transitional stage to HCC and use evidence-based surveillance and management measures.
Regular ultrasound screening and suitable treatment options like liver transplantation, ablation, or systemic treatment can significantly affect the patient outcomes of the disease, as it can be caught early. It is very important to stress prevention by vaccination, antivirals, and lifestyle changes that help overcome the progression of cirrhosis and the development of HCC.
Through being aware of the changing guidelines and innovations, clinicians will be at a vantage point to deliver better care and minimize the burden of hepatocellular carcinoma in cirrhotic patients.
The source of this article is DR Gina Sam MD






